Every day, the danger of antibiotic resistance is gaining more attention in the media.
Finally, the scientific community and medical industry are realizing that our global dependence on antibiotics – prescribed by doctors, flooding our household products, and even injected into our food supply – could be a bad idea in regards to long-term fighting of infection.
What is Antibiotic Resistance?
Simply put, antibiotic resistance occurs when a bacteria, virus, fungus, or parasite survives the effect of the standard antibiotic, antimicrobial, or antiviral drug used to control them.
It’s a matter of evolution.
Germs that were treated effectively with antibiotics have mutated, developed an immunity to the drugs that once killed them, and they can pass their resistance on to the next generation of germs.
Here are a few of the known diseases slowly gaining antibiotic resistance:
- Methicillin-resistant Staphylococcus aureus (MRSA) – commonly known as staph infection and the majority of cases are contracted in a healthcare setting
- Meningitis – a bacterial illness that affects primarily children and young adults
- Salmonella – a bacterial infection resulting from food contamination
- Tuberculosis – the most prevalent infectious disease worldwide; affects the lungs
- Influenza – contagious respiratory virus
- Candida – yeast infections which can affect various areas of the body
- Malaria – parasite that is transmitted by mosquitoes; more than half the world’s population is at risk for malaria and it caused more than 600,000 deaths in 2012. The majority of those deaths were children under the age of five.
As a result, what were once considered “simple” infections and illnesses – easily treated with a prescription or a shot – no longer respond to medication used heavily over the last eight decades. Urinary tract infections (UTIs), pneumonia, diarrhea, and skin or blood infections are the most common results of antibiotic resistant germs.
I’ve written about many of these antibiotic resistant “superbugs” in my groundbreaking book World Without Antibiotics, in particular because the world at large is at risk if we do not halt our overuse of antibiotics.
The Center for Disease Control and Prevention (CDC) calls antibiotic resistance “one of the world’s most pressing public health problems.” We are considered at a “crisis point” by the CDC, the World Health Organization (WHO), Infectious Diseases Society of America (IDSA), and virtually every other global organization that tracks disease and treatment.
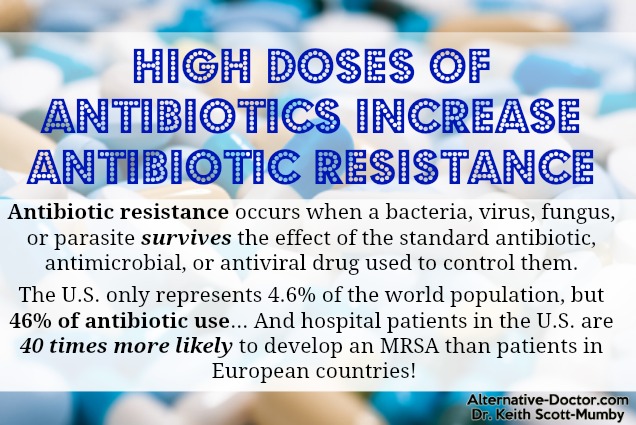
The United States represents 4.6% of the world population and 46% of antibiotic use.
If you want to understand how little value you have to the pharmaceutical companies, consider this: the last commercial antibiotic was developed forty years ago and Big Pharma refuses to make anymore because they don’t see a big enough return on their investment.
To make matters worse, the Food and Drug Administration (FDA) has non-working guidelines (according to experts in countless health organizations) on the clinical trials for antibiotics – making it almost impossible to bring new drug therapies (profitable or not) to market.
The real money to be made is in mood regulating drugs for depression and anxiety…not antibiotics. Therefore, when bacteria, viruses, fungus, and parasites become resistant to available antibiotics on the market today, there are no new ones being developed.
Why You Should Worry About Antibiotic Resistance
According to the National Institutes of Health (NIH), every year approximately 5-10% of patients develop a hospital-acquired infection (HAI).
In 1992, deaths attributed to HAIs were just over 13,000 per year. Today, more than 90,000 patients die annually as a result of a hospital-acquired infection that is resistant to standard antibiotic treatment.
Hospital patients in the United States are as much as 40 times more likely to develop an MRSA than patients in European countries.
Researchers at Oxford discovered another cause for serious concern. In their study, published in Molecular Biology and Evolution, they explained the danger of cross-resistant bacteria. Those are bacteria which are resistant to one form of antibiotic or antimicrobial that show resistance to other forms as well. This could drastically shorten the list of treatment options for some patients.
6 Ways to Minimize Antibiotic Resistance in Everyday Life
- Stop unnecessary antibiotic use for yourself and your children. Never take antibiotics (or ask them to be prescribed) for viral colds, flus, coughs, or sore throats. Experts estimate that 70% of antibiotic prescriptions are unnecessary and lead to antibiotic resistance.
- Discard unused antibiotics. Prescriptions lose potency over time and taking ineffectual antibiotics can lead to drug resistance. Take the full dose as prescribed and always ask for the shortest course available. Studies have shown that taking antibiotics for fewer days are just as effective.
- Never take antibiotics that are not prescribed to you. Killing “some” of the bacteria is an excellent way to mutate those that remain. Do not self-treat and assume that you require an antibiotic, especially not one that you haven’t been personally prescribed.
- Wash hands thoroughly. Skip the antibacterial soap varieties. Simply wash your hands for thirty seconds with standard hand soap for the same result without exposing yourself to unnecessary antibacterial compounds through the pores of your skin.
- Avoid antibiotics in your food supply. Buying organic where possible is an excellent way to cut many of the food source antibiotics from your diet.
- Adopt healthy lifestyle choices. Good nutrition, exercise, proper hydration, and plenty of sleep may sound “old school” – but they work. Avoiding antibiotic resistance starts by doing everything you can to not get sick in the first place.
The first step of stopping antibiotic resistance and the spread of superbugs starts with YOU.
This is not a “Chicken Little” situation. This is a real and growing issue in every country in the world. If left unaddressed, it could conceivably lead to a day when patients once again succumb to illnesses that claimed the lives of millions before the discovery of antibiotics.
Pharmaceutical companies say there is no money to be made in developing new antibiotics – so steeling yourself against antibiotic resistance is up to you, every individual, and me before it is too lat
The post High Doses of Antibiotics Increase Antibiotic Resistance appeared first on Dr. Keith Scott-Mumby.
