Honestly, this is one of the BIGGEST “I told ‘ems!” of my career.
Let me explain that phrase for the many newcomers. An “I told ‘em!” is where I said it years or DECADES before it was accepted by the medical profession. I’ve had many dozens of these over the years, from low-dose sublingual desensitization (SLIT, you can Google it!), to brain allergies; from ambient xenobiotic chemicals sensitizing individuals to foods, to finding migraine is 95% food allergy.
I said it and I knew I was right. It just took “science” a long time to catch up. In the interim, I’ve been called a crook and a fraud, a charlatan and quack. They called my food allergy stuff “Mumby-Jumbo” at the local hospitals in my city.
Do you think when I was eventually proven right that I got any apologies or withdrawals of criticism? Ha!
The case in point today is about chronic fatigue syndrome (CFS). So, what is chronic fatigue syndrome? When I joined the forming clinical ecology movement in the 1970s, we talked about “tension-fatigue” syndrome. It summarized well the main points of the condition (stress, misery and a dragging fatigue).
Note, we did not assign any cause; it was a clinical syndrome, meaning you can find the complaint but without necessarily being able to explain it. Mainstream doctors don’t like that. It smacks of patient hypochondria. It must have a “proper” name and be in the textbooks for it to be a “real” disease.
If not, the patient is faking it.
Like my colleagues (just a handful of us around the world in those days), I had a steady succession of miserable patients who had been scorned, derided and insulted by the profession that was supposed to help them find comfort and a cure. Many were referred as psychiatric patients because, if their complaint was not in the medical textbooks, it was clearly a delusion. Maybe they were making it all up, because they were “inadequate” or “wanted attention”?
I ask you, what in the name of science was that all about?
As revolutionary experts in food allergies and environmental chemical sensitivity, my pioneering colleagues and I soon learned that these patients responded to our overload approach. Most got well very quickly, utterly disproving the theory that the patient wanted to be sick or was using the complaint for some self-serving reason.

Then, in the early 80s, we began to notice this condition often came on strongly after a viral illness. So we began to talk of post-viral fatigue syndrome. Coxsackie B infection fell under suspicion. I actually engaged with the Professor of Pathology at a local path lab and collected blood specimens from my patients, which he had analyzed. Nothing conclusive found.
The Epstein-Barr also got the blame. Again the maverick—even amongst my own people—I was already writing that ANY viral illness could do this. I also had a section on “smouldering virus” in my 1980s books, which today we would call “stealth pathogens”.
The truth is, it’s not possible to tie in any one cause and those who call it EBV or “Lyme” are just plain wrong. These conditions mimic the chronic fatigue condition often but are not “the” cause. It’s multifactorial; parasites, food allergies, nutritional deficiencies, chemical overload and, yes, psychology factors all play a part.
I was even beginning to write about a “flat” immune system, resulting in extra food and chemical sensitivities. I speculated in one book (1988) that maybe people were getting the viruses because their immune systems were goosed, rather than the other way round. Having seen what toxic overload does to immunity and allergies, it was (and still is) a very plausible line of enquiry.
Exercise Triggers The Pains
There continued a furor over this ‘fake’ illness for many years. I remember when, around 1984, when the World Health Organization (WHO) declared it was a real disease, that most doctors rejected this idea as rubbish and would not, in their arrogance, accept that the patient was truly unwell and medical incompetence at diagnosis and treatment was the issue.
One of the curiosities of the complaint I’m writing about was that exercise produces severe deterioration in the patient’s ability to function (called post-exertional malaise). The old idea of “pull yourself together and go for a good, stiff walk…” was ruinously stupid advice. Yet doctors continued to believe this sort of good talking to was the answer to the patient’s reluctance to live a normal life.
In the UK (because we like fancy classical language), we eventually settled on the term myalgic encephalomyelitis or ME. Myalgic means pains in the muscles; encephalo- means the brain is involved; and myelitis means the nerve trunks are involved.
In the USA, the same complaint was called fibromyalgia, which is an inadequate name. It means only “aches and pains”. I prefer the term ME.
An interesting historic name for it was neurasthenia (nervous weakness) and its most famous sufferer was Charles Darwin. He was incapacitated for days at a time. His symptoms just shriek of food allergies:
…malaise, vertigo, vomiting, cramps and colics, bloating and nocturnal intestinal gas, headaches, severe tiredness, nervous exhaustion, dyspnea, skin problems such as blisters all over the scalp and eczema, crying, anxiety, fainting and tachycardia. [Wikipedia]
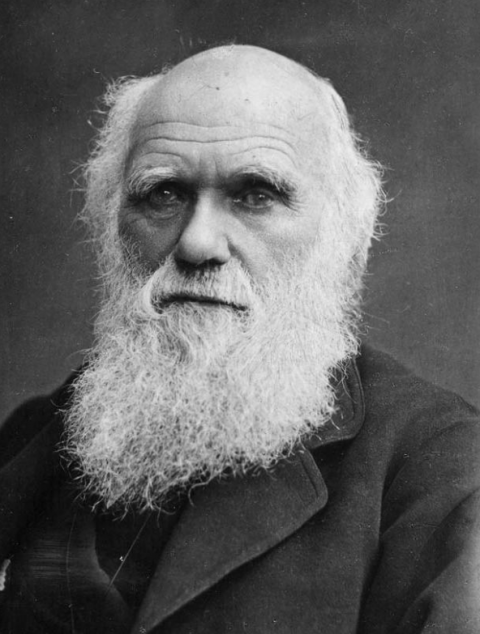
Charles Darwin, possibly an ME sufferer
What Is Chronic Fatigue Syndrome? Real At Last
Now, it’s suddenly real and a 235-page report from the Institute of Medicine entitled “Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness” (published online February 10, 2015) insists ME is a “serious, complex, multisystem disease” that physicians need to view as “real” and diagnose.
Hooray! Just 30 years late!
“The central point is that ME/CFS is a diagnosis to be made,” according to the IOM’s report. Unfortunately, in reflection of the condition’s hallmark defining symptom, post-exertional malaise, the report proposes a new name be adopted, “systemic exertion intolerance disease (SEID).”
I strongly disapprove of new and unnecessary terminology.
“It’s time to stop saying that this is a just figment of people’s imagination. This is a real disease, with real physical manifestations that need to be identified and cared for,” according to Committee Chair Ellen Wright Clayton, MD, JD, professor of pediatrics and director of the Center for Biomedical Ethics and Society at Vanderbilt University, Nashville, Tennessee.
Panel member Peter Rowe, MD, professor of pediatrics and director of the Chronic Fatigue Clinic at Johns Hopkins Children’s Center, Baltimore, Maryland, told Medscape Medical News, “This is an illness that can have a profound impact on people’s function, their ability to maintain their jobs or continue their education. This was very clear from the evidence that the committee reviewed.”
In particular, the panel found sufficient evidence linking the illness to immune dysfunction, especially diminished natural killer cell function, and viral infections, particularly Epstein-Barr virus.
The report does not advise that clinicians routinely perform expensive testing that was done in some of the studies. Instead, the diagnosis should be primarily based on appropriate history, physical examination, and targeted symptom-based workup.
How Common Is It?
This will scare you: according to the report an estimated 84% to 91% of sufferers are not yet diagnosed.
The report’s final chapter outlines a broad plan for disseminating the new criteria, including outreach to professional organizations representing adult and pediatric primary care, obstetrician-gynecologists, emergency medicine practitioners, psychologists, psychiatrists, rheumatologists, gastroenterologists, sleep medicine specialists, infectious disease practitioners, and cardiologists.
The 15-member writing panel, consisting of experts and non-experts in the field, based their conclusions on a comprehensive literature review; testimony from patients, clinicians, and researchers during public hearings held in January and May of 2014; and almost 1000 public comments.
According to Dr Rowe, “It was a unanimous committee report…. It was interesting for us who are clinicians in the field to see how obvious the direction of the evidence was for those who are scientists, but not specialists in this area.”
Well, that’s that then. After more than 30 years, CFS or ME has finally landed. I am deeply grateful for the progress, albeit a teeny bit slow!
Note: The report was sponsored by the Office of Women’s Health in the Department of Health and Human Services, the National Institutes of Health, the Centers for Disease Control and Prevention, the US Food and Drug Administration, the Agency for Healthcare Research and Quality, and the Social Security Administration.
The post What Is Chronic Fatigue Syndrome? When Fatigue Is More Than Just Tiredness appeared first on Dr. Keith Scott-Mumby.

